I’ve spent years watching patients react to the news that they have calcium buildup in their coronary arteries. The initial confusion is always the same—”Wait, isn’t calcium supposed to be good for you?” Well, yes and no. Calcium keeps your bones strong, but when it starts accumulating in your heart’s blood vessels, that’s a different story entirely.
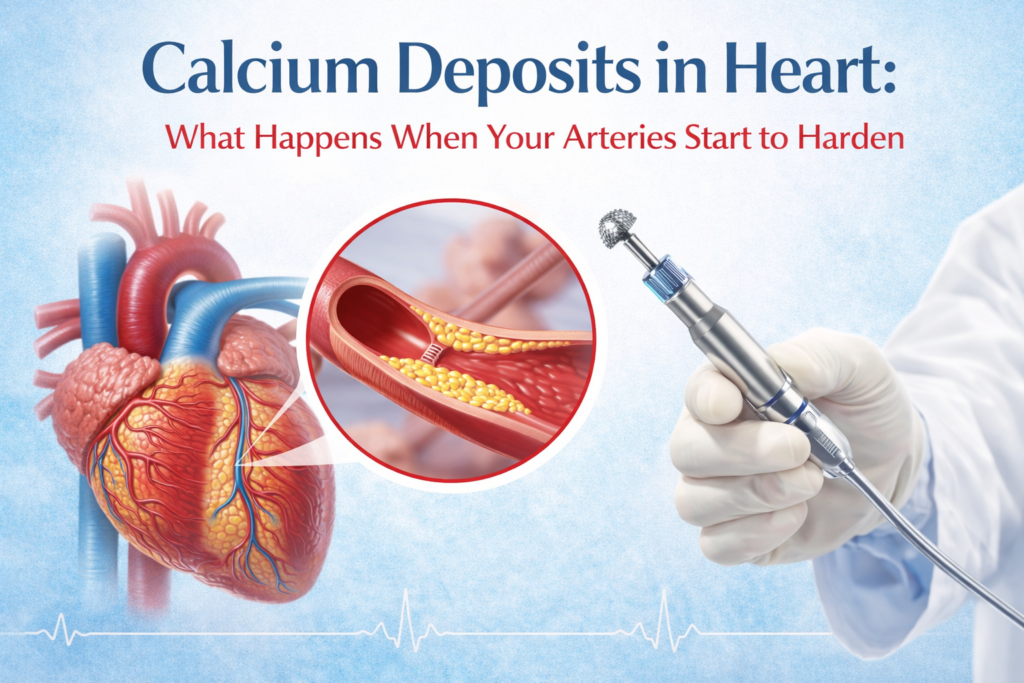
Think of it this way. Your arteries are meant to be smooth and flexible, like garden hoses that can expand and contract as needed. When calcium deposits form along the artery walls, they create hard, rigid patches that can’t bend. Over time, these patches grow, narrowing the space where blood needs to flow. And that’s when problems start.
Why Does Calcium Build Up in the First Place?
Here’s what surprises many people: calcium deposits in heart arteries aren’t just random. They’re actually your body’s misguided attempt to repair damage.
When your artery walls get injured—from high blood pressure, smoking, high cholesterol, diabetes, or just decades of wear and tear—inflammation kicks in. Your body tries to patch things up, and calcium gets deposited as part of this healing response. Unfortunately, instead of fixing the problem, it creates a new one. The calcium hardens into what doctors call plaque, and this plaque makes your arteries stiff and narrow.
Age plays a huge role here. The older you get, the more likely you are to develop some degree of heart calcification. Men typically start seeing this in their 40s and 50s, while women often develop it a bit later, usually after menopause. But I’ve also seen younger patients with severe calcium buildup, especially if they have strong family histories or uncontrolled risk factors.
The Real Risks You’re Facing
Calcium deposits don’t just sit there doing nothing. As they grow, they reduce blood flow to your heart muscle. Less blood means less oxygen, and your heart doesn’t function well when it’s starved for oxygen.
In practice, patients start noticing chest pain during physical activity—that’s angina. Some describe it as pressure or tightness, like someone’s sitting on their chest. Others feel it more as a dull ache that radiates to their jaw or left arm.
But the bigger concern? Heart attacks. When severely calcified plaque ruptures or a blood clot forms on top of it, blood flow can stop completely. That’s a medical emergency. Even without a full blockage, severe calcification increases your risk of heart failure, irregular heart rhythms, and sudden cardiac events.
What makes heavily calcified arteries particularly tricky is that they’re hard to treat with standard procedures. You can’t just inflate a balloon in there and expect it to work—the calcium is too rigid.
When Standard Treatments Hit a Wall
Most people have heard of angioplasty—the procedure where doctors thread a tiny balloon into a blocked artery and inflate it to widen the passage. They usually place a stent afterward to keep things open.
That works beautifully for soft plaque. But when you’re dealing with rock-hard calcium deposits? The balloon often can’t expand properly. It’s like trying to inflate a balloon inside a pipe made of concrete. The calcium just won’t budge, and sometimes the balloon can’t even reach the right pressure to make a difference.
This is where things used to get complicated. Surgeons would have to consider bypass surgery, which is major open-heart surgery with a longer recovery. But now there’s another option that’s changed the game for many patients.
How Rotational Atherectomy Works
The rotational atherectomy procedure is essentially a specialized drill for your arteries. I know that sounds intense, but stay with me.
Doctors guide a thin catheter through your blood vessels to the calcified blockage. At the tip of this catheter is a tiny, diamond-coated burr—shaped like a football and no bigger than the head of a pin. This burr spins at incredibly high speeds, somewhere around 140,000 to 180,000 rotations per minute.
As it spins, it grinds the hard calcium deposits into microscopic particles, much smaller than red blood cells. Your body’s natural filtration system handles these tiny particles without issue. The key here is that rotational atherectomy doesn’t remove all the plaque—it creates channels through the calcified areas and makes the artery more flexible again. This allows the balloon and stent to do their job afterward.
The whole thing is done through a small puncture in your wrist or groin, not open-heart surgery. Most patients are awake but sedated during the procedure.
What Patients Actually Experience
Recovery from rotational atherectomy is surprisingly quick for what’s being accomplished. You’re typically in the hospital for a day or two, mainly for observation. There’s some soreness at the catheter insertion site, but nothing like recovering from bypass surgery.
People often notice improvement in their symptoms within days. That crushing chest pain during walks or climbing stairs? It starts to fade because blood can flow more freely again. One patient told me he could finally play with his grandkids without having to stop every few minutes. These are the moments that make the procedure worthwhile.
Of course, it’s not a permanent fix for everyone. Calcium can build up again, especially if underlying risk factors aren’t addressed. That means medications, lifestyle changes, better diet, exercise—the whole package matters.
Is This Right for You?
Not everyone with calcium deposits needs rotational atherectomy. Doctors typically reserve it for severe cases where the calcification is so extensive that standard angioplasty won’t work. Your cardiologist will look at imaging studies, assess how much calcium is present, where it’s located, and how it’s affecting blood flow.
If you’re dealing with heart calcification, the conversation with your doctor should cover all options—from medication management to this procedure to surgery if needed. Every case is different. Some people do perfectly fine managing their condition with drugs and lifestyle modifications. Others need intervention.
What matters most is catching it before a crisis happens. Regular checkups, especially if you have risk factors, give you options. By the time you’re having severe symptoms or a heart attack, your choices become more limited and urgent.
The good news is that techniques like rotational atherectomy have expanded what’s possible for treating even the toughest blockages without major surgery. That’s progress worth noting.